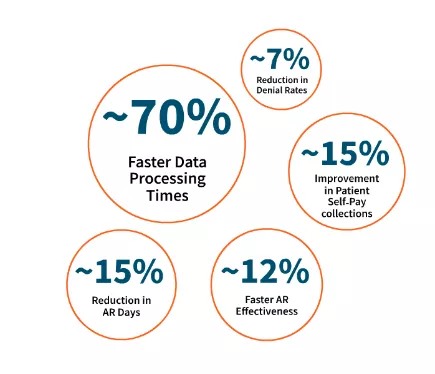
Improve financial outcomes using data-driven insights
At EXL Health, we know that accelerating revenue capture and protecting working capital is more important than ever. That’s why we look and go deeper to help improve revenue capture, optimize payment processing, and maximize and protect working capital.
How? By combining our deep domain expertise, analytics-driven insights, and cutting-edge technologies.
EXL x REVELOHEALTH
The integrated revenue management solutions have been developed in collaborative partnership with REVELOHEALTH, delivering a comprehensive, data-driven payment processing and revenue analytics capability to help providers optimize revenue cycle management. This solution seeks to aggregate and homogenize patient data from a variety of sources through independent repricing services, revenue cycle management services, payment analytics, and advisory services.
Download brochure






