Savings, efficiencies & innovation delivered to top-tier health plan
Challenge
A large national healthcare insurer was looking to take their Utilization Management (UM) operations to the next level. They sought a strategic partner that would bring innovations, efficiencies and savings to their organization and help them deliver continuous process improvements.
The health plan’s current UM intake operations relied on a large number of staff, yet UM performance consistently ran flat.
Additionally, due to the competitive nature and shortage of the clinical staffing environment, the health plan needed a partner who demonstrated deep staffing capabilities to avoid disruptions to clinical operations.
The client recognized an immediate need for improved Utilization Management performance, and decided it was time for change. Critical to the success of their Clinical Services business, the health plan needed a partner who could not only deliver Utilization Management domain expertise, but also demonstrated market leadership in analytics, technology, and innovation embedded within delivered services and workflows.
Human Ingenuity in Action
After selecting EXL Health as their partner, the EXL Health Process Excellence team got to work analyzing the health plan’s overall UM operations. Through this analysis, approximately 30% efficiency was identified across several key opportunities through digital enablement and lean six sigma projects.
Once staffing requirements were defined, EXL Health initiated and executed the recruitment, training and equipping of both clinical and nonclinical team members.
Through EXL’s proprietary Healthcare Academy, nearly 600 domain experts were prepared with the in-depth, specialized skills needed to deliver efficient and accurate services to the health plan. Due to the level of deep domain training and education provided, including the ability to certify Philippine-based nurses as USRNs, EXL Health is able to operate above the competitive staffing environment and ensure staffing shortages do not disrupt operations.
Utilization Management Operations Deliver Quality & Efficiency
Today, EXL Health is delivering Utilization Management intake services across the plan’s entire book of business, including Commercial, Medicare and Medicaid members. These services are delivered out of four locations, including three Philippines delivery centers (Manila, Alabang, and Cebu) and one center based in Pune, India.
With over 300 in-house domain experts, EXL Health receives authorization requests through telephonic and fax methods, then manages functions including opening cases, authorization status check, benefits and eligibility check, and routing to the appropriate clinical area for medical review.
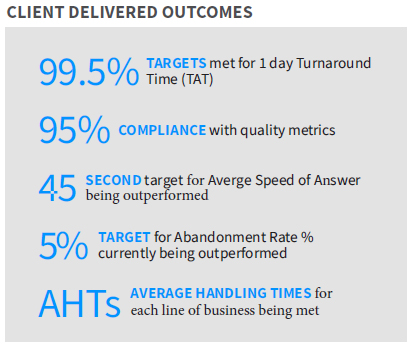
EXL Health is consistently meeting the health plan’s quality and care model performance standards and is currently handling over 4,000,000 requests annually through both modes of intake.
Post-Service Validation of Medically Necessary Services
To further support overall Utilization Management process, EXL Health also delivers post-payment utilization review services for health plans. This is an extension of pre-payment operations, to assure that members receive medically-necessary health care services and that the claims for these services are submitted properly.
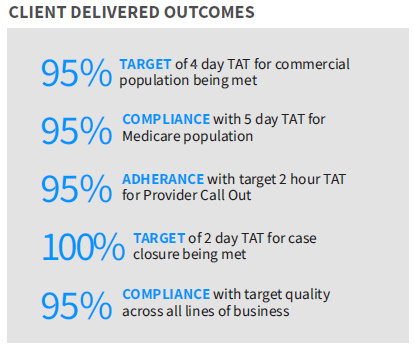
EXL Health has nearly 150 US Registered Nurses (USRNs) who review Commercial and Medicare post-service clinical claims sent by the providers for all inpatient and outpatient services. The USRNs review claims for approval or denial, based on industry-standard clinical guidelines. They route cases to appropriate clinical areas for additional review, working with post clinical reviewer opposing decisions. The team also works directly with providers to collect additional information if needed to make approval or denial decisions.
Looking Ahead to Automation & Innovation for Greater Outcomes
 With optimized operations hitting target performance metrics, the health plan is exploring how applying automation and innovation can create greater efficiencies and savings. Innovation – such as digital voice automation solutions, including Interactive Voice Response (IVR) – can deliver significant reductions in cost of services and impacts on member experience and satisfaction.
With optimized operations hitting target performance metrics, the health plan is exploring how applying automation and innovation can create greater efficiencies and savings. Innovation – such as digital voice automation solutions, including Interactive Voice Response (IVR) – can deliver significant reductions in cost of services and impacts on member experience and satisfaction.
With over 300 in-house domain experts, EXL Health receives authorization requests through telephonic and fax methods, then manages functions including opening cases, authorization status check, benefits and eligibility check, and routing to the appropriate clinical area for medical review.
EXL Health is bringing its deep investments in digital, analytics and innovation to the health plan’s cutting-edge technologies, helping deliver continuous process improvement and greater outcomes across healthcare businesses.
