The challenge
Summarizing medical records for insurance, legal, and healthcare purposes can be complicated due to:
Steep processing costs
Medical summarization expenses are 40% higher when performed by adjusters and paralegals. Often these professionals are excellent at their core jobs but struggle with medical record summarization and evaluations.
Unfamiliar terminology
Even neatly prepared records can contain perplexing medical jargon and abbreviations. Professionals often have a limited understanding of medical conditions, leading to inaccurate conclusions.
Disorganized, incomplete records
Medical records typically arrive unsorted, disorganized, in duplicates, and often include unrelated documents. Collating and organizing records can be very time-consuming.
What we do
MedConnection™ is a Human AI collaboration tool, helping to bring
- Workforce having 600+ hours of experience in managing medical/ legal document extraction
- NLP based extraction models trained by 10M+ medical documents
- Agile platform to help seamlessly ingest documents & provide extremely user friendly human validation UI layer
to deliver precise, succinct clinical insights/ summaries efficiently
How MedConnection™ and Swift by MedConnection™ can help
MedConnection™ uses an expert-led approach to quickly read medical records and produce an accurate summary of diagnoses, conditions, treatments received, and bills incurred.
Swift by MedConnection™ approaches medical review in a similar way using generative AI to produce reports while supported by an expert-in-the-loop review.
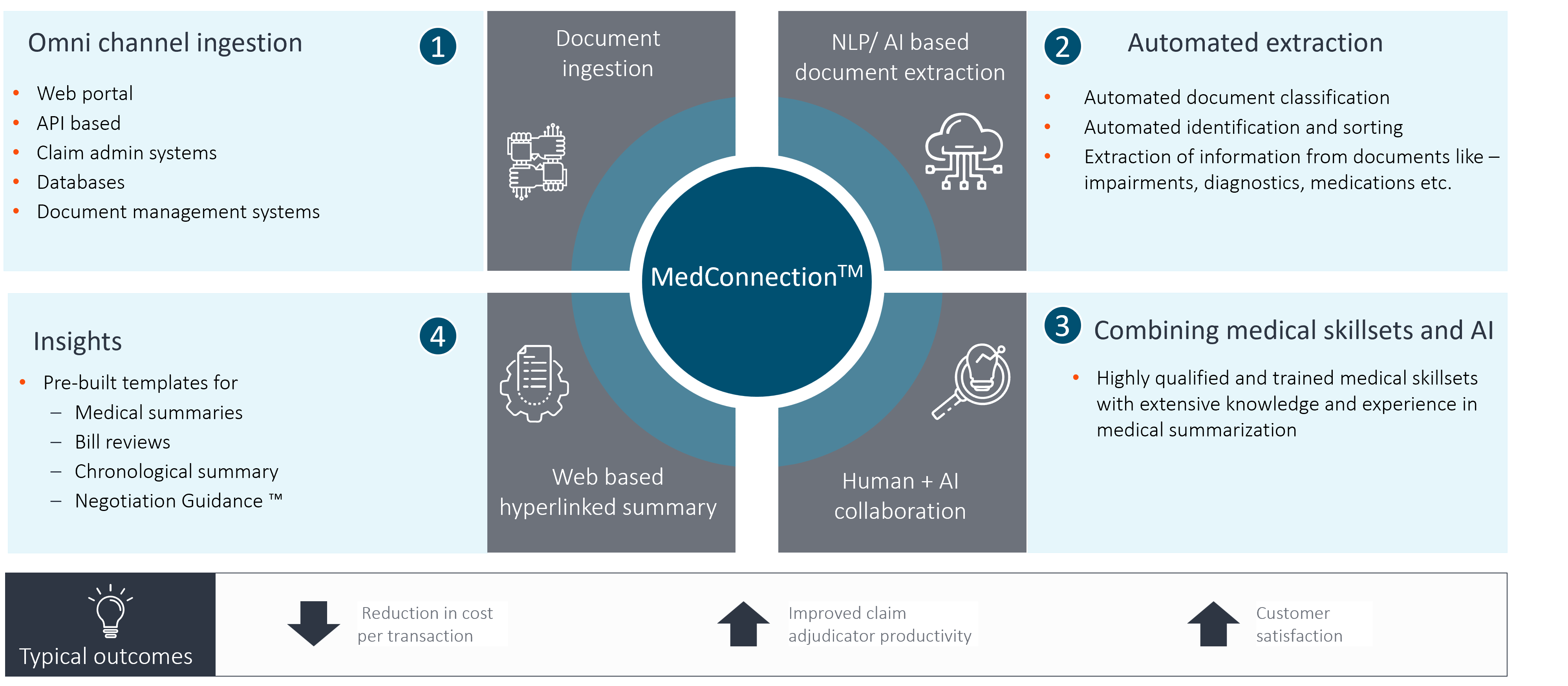
Pillars of MedConnection™ and Swift by MedConnection™
Swift by MedConnection™ uses generative AI to recognize, deduplicate, sort, and extract relevant information from documents. It untangles the mess to accelerate the settlement of your claim or case.
MedConnection™ generates customized negotiation points based on the facts extracted from the medical records. These points can drive negotiations and lead to an optimal case or claim settlement.
Our team of doctors, nurses, and other medical professionals have decades of experience reading and interpreting medical records. They are the seasoned guides for achieving a thorough understanding of your case or claim.
Both MedConnection™ and Swift by MedConnection™ offer flexible document ingestion through web portals, APIs, scanning stations, databases, and other document management systems.
Benefits
75%
Improvement of turn-around times

Highly accurate
summaries
40%-80%
Cost reduction
MedConnection™ and Swift by MedConnection™ Solution Overview
Human-AI collaboration platform, combining experienced medico skillsets and Generative AI models to generate accurate clinical insights
Effective negotiations supported by MedConnection™
![]() Our claims organization has realized benefits through the use of MedConnection’s ™ Negotiation Guidance™ tool. It equips adjusters with clear, structured talking points when engaging with attorneys or pro se claimants. Providing a quick reference to key claim factors, it helps adjusters maintain consistency in their discussions, leading to more effective negotiations. The tool not only supports informed decision-making, but also fosters more productive and fact-based settlements, ultimately contributing to a smoother claims resolution process.
Our claims organization has realized benefits through the use of MedConnection’s ™ Negotiation Guidance™ tool. It equips adjusters with clear, structured talking points when engaging with attorneys or pro se claimants. Providing a quick reference to key claim factors, it helps adjusters maintain consistency in their discussions, leading to more effective negotiations. The tool not only supports informed decision-making, but also fosters more productive and fact-based settlements, ultimately contributing to a smoother claims resolution process.![]()
Claims executive at a leading mutual insurance organization
Discover how a major US retailer saved $5.5M with AI-driven innovation
See how one of the nation’s largest retailers tackled inefficient processes, reduced legal costs, and achieved a 4:1 ROI in just one year. Learn how the AI-powered MedConnection™ streamlined medical reviews, improved quality to over 98%, and delivered robust insights that saved millions.