Let’s partner your way to address your unique payment integrity challenges
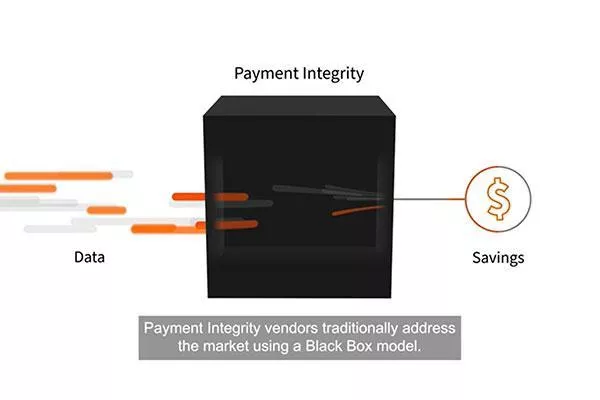
At EXL Health, we believe in a modular approach to payment integrity, allowing our customers to access vendor software, analytics, people, and processes to transparently identify and address overpayments, trends, and unique business challenges. Our innovative approach provides payers deeper insights into their payment integrity program through transparent and accessible information. Whether looking for a traditional solution or components within a modular delivery model, we partner with our clients to help make healthcare transformation happen.
Get solution sheetWhat we do
EXL helps payers improve reimbursement by providing insights to control costs, reduce expenditures, and optimize revenue.
Awards and recognition
Spotlight on achievements in excellence
Proven outcomes: human ingenuity at work
One of our long-standing payer clients was looking to streamline their payment integrity program, specifically their diagnosis-related group (DRG) auditing solutions. As their most trusted and first-pass post-pay vendor for DRG coding and clinical auditing services, they approached EXL when looking to reduce vendors to decrease administrative and operational workloads within vendor management. Leveraging human ingenuity, technology, and analytics-enabled solutions, EXL’s payment integrity solution was able to impact payment accuracies, cost management, and quality outcomes – all key to value-based performance success.
By partnering with our client to better understand their needs and implement custom solutions, EXL Health was able to create significant value to the organization, yielding an improved savings rate of 120% within 2021 and 2022.
- 56% overall DRG savings for client in 2021
- Expected continued growth in 2022
- Improved resource efficiency due to streamlining from a singular vendor