EXL Health leads the way to provide payment integrity for telehealth claims
Major healthcare payer achieves significant cost savings using specialized data-driven auditing program for high-volume, low-dollar claims
The healthcare payer realized this wave of expense was headed into their system and they lacked adequate billing and cost containment capabilities specific to telehealth.
Challenge
A large U.S. healthcare payer that offers healthcare benefits to millions of members was looking to address waste and abuse for its telehealth claims. EXL Health has a long-standing relationship with this client and was already providing payment integrity services for the payer’s inpatient and outpatient claims to identify overbilling and overpayment.
Historically, telehealth services in the U.S. were not uniformly available by healthcare providers nor used consistently by patients. In March 2020, the widespread crisis of the COVID-19 pandemic immediately and drastically changed the telehealth industry. Congress enacted major changes to Medicare rules regarding how telehealth could be used and what would be reimbursed. In turn, healthcare payers followed Medicare’s lead regarding telehealth services to keep the U.S. healthcare system up and running during an extended period of social isolation.
The use of telehealth services grew dramatically in the first year of the pandemic. According to the U.S. Department of Health and Human Services Office of the Inspector General (HHS-OIG), “more than 28 million Medicare beneficiaries—about 2 in 5—used telehealth services that first year. In total, beneficiaries used 88 times more telehealth services during the first year of the pandemic than they did in the prior year.”
For EXL’s client, the healthcare payer saw a significant rise in billing claims for professional services telehealth sessions, a trend that gave the client pause, as studies have shown telehealth claims as prone to fraud, waste and abuse. Even before the pandemic, five telehealth companies in 2019 were charged as part of one of the largest health care fraud schemes investigated by the FBI and HHS-OIG, involving more than $1.2 billion in loss.
The healthcare payer realized this wave of expense was headed into their system and they lacked adequate billing and cost containment capabilities specific to telehealth. The payer turned to EXL Health to devise a telehealth payment integrity program to determine whether their providers were billing for telehealth services appropriately.
Human Ingenuity
Working as a collaborative partner, EXL Health created a payment integrity program specific to telehealth claims, starting with a proof-of-concept project. Focusing on high-level claim data provided by the payer, the EXL Health team conducted a random sampling of 1,000 professional telehealth claims. The project was based on nationally accepted standard coding guidelines combined with the payer’s specific policies.
The team leveraged its proprietary analytics technology combined with best-in-class clinical reviews to identify anomalies and outliers on provider behaviors. EXL Health collaborated with various internal teams to offer the client auditing services, data-driven analytics, reporting, and guidance from subject matter experts. A key factor to EXL’s success was its strong client partnership and the ability to be nimble and flexible to accommodate the payer’s needs. Through this work, the EXL Health team has helped the payer to mitigate overpayments, maximize savings and provide opportunities to educate providers on to correct billing behaviors specific to telehealth claims.
Due to the success of the pilot program, the EXL Health team has expanded the project to a wider scope to include more professional providers along with behavioral health providers to identify and address overpayments, trends, and payer-specific business challenges.
Results
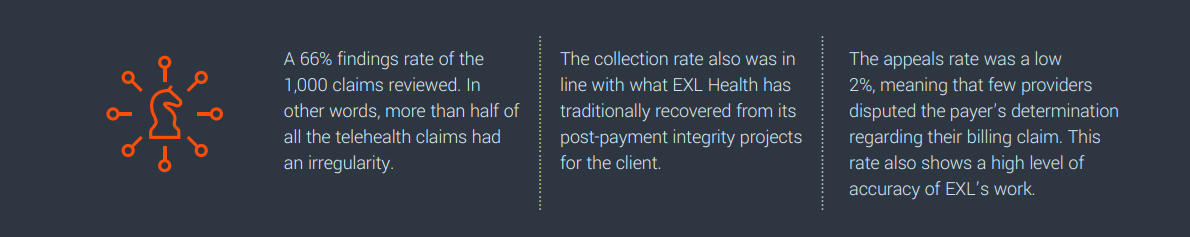
EXL Health’s pilot program of the payer’s telehealth claims produced clear and compelling results:
Finding a successful formula for auditing telehealth claims has been elusive for most healthcare technology companies because telehealth claims are high in volume, but low in per provider cost. Yet the need for payment integrity specific to telehealth has never been greater. Today, telehealth is one of the largest and fastest growing segments of healthcare. The U.S. telehealth market size was valued at USD 23.5 billion in 2021 and is expected to expand at a compound annual growth rate (CAGR) of 44.4% from 2022 to 2028.
EXL Health is one of the first healthcare technology companies that has succeeded in addressing payment integrity specific to telehealth claims. Future plans for the telehealth payment integrity program include establishing a process that identifies high-risk providers for potential fraud and moves them into a pre-pay audit program. Moving claims to pre-payment eliminates the payer’s time and expense needed to claw back money from fraudulent claims already paid out and benefits providers upfront by decreasing the administrative burden in a post-pay environment.
3. U.S. Telehealth Market Size, Share & Trends Report, 2030 (grandviewresearch.com)
