Digital intake solution for insurance
The insurance industry spends countless hours and billions of dollars on capturing information from more than 3B documents and rekeying data into multiple downstream systems. From 5 to 10% of enterprise bandwidth and related costs are engaged in the processing of content, which could benefit from document automation.
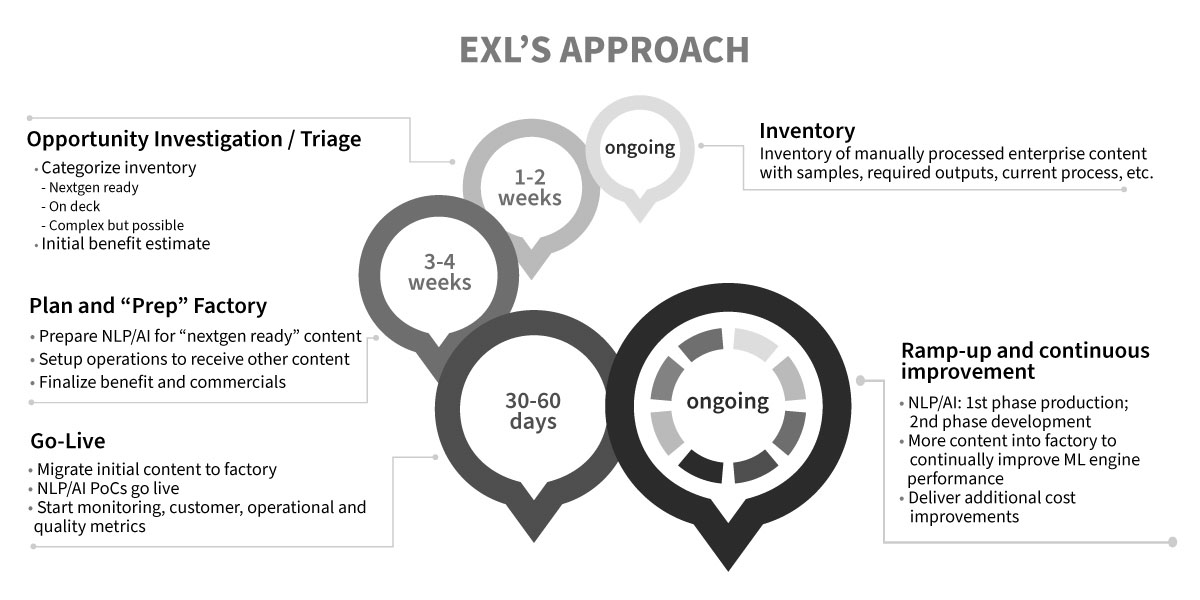
EXL’s Digital Intake solution is a key enabler to drive a contactless experience and a catalyst to unlock value from document automation, analytics, and AI-based digital transformation. Insurers can improve their customer experience with greater savings. We have seen an improvement of automation throughout by up to 70% straight-through processing, resulting in improved customer experience and savings.
What we do
EXL has developed a machine learning-based Digital Intake solution for insurance that blends the experience and knowledge of high-performing employees with the precision and effectiveness of a well-oiled machine. Today, smart digital intake solutions are improving customer experience, reducing operating costs, accelerating digital transformation, and maximizing operational resiliency across business functions. As machine learning models continue to evolve, we find the best results are coming from narrowly defined use cases, such as underwriting, claims processing, and policy maintenance, to yield rapid results. EXL’s solution is tailored to business requirements through leveraging a combination of tools and technologies instead of a specific, off-the-shelf product that might not yield best results in different business contexts.

Improve customer experience

Reduce operating cost

Enable digital transformation

Build resiliency
Proven outcomes
Across several large insurance clients, EXL was able to deliver the below sampling of delivered value and results
Our vlaues
How is EXL's Digital Intake different?